Under the Funding Microscope
Here’s What You Need To Know
The temperatures may be high, but the investment climate is staying cool. Nowhere is this reality more evident than in the life sciences and biopharmaceutical industries. In March, Delve’s Life Sciences Outlook 2023 explored why the post-pandemic operating environment is starkly different than the one in 2020 and 2021, and as the year unfolds, the headwinds continue to grow. That reality has implications for a range of industries.
While venture capital and private equity firms have plenty of capital, they are being highly judicious in deploying it. Economic indicators and rising interest rates are certainly part of their calculation, but when it comes to life sciences – and a number of other sectors – the policy direction from Washington is also putting many early-stage firms under a more rigorous microscope as investors increasingly consider not only where and when to invest, but even if. Here’s what public affairs professionals need to know to help their organizations stand firm amidst the economic and political headwinds.
An “Investment Plateau” Has Early-Stage Firms Scrambling For Viability
The life sciences and biopharma boom brought on by COVID-19 saw outsized valuations and unprecedented investment in the industry. While there is still good news related to long-term and sustainable growth, industry experts see an “investment plateau.” More cautious investments, combined with ramped-up regulatory oversight, has resulted in a 40% drop in early-stage investments and a 30% drop in venture capital funding. The decline in early-stage investments has meant layoffs and shifted firms’ focus on “nearest-term value drivers” rather than long-term innovation. As SVB’s Healthcare Industry Trends Mid-Year 2023 Update notes, “valuations are being recalibrated to align with current market conditions, rooted in fundamentals such as clinical assets and paths to profitability.”
For public affairs and government relations professionals, this shift in the funding environment requires an increased focus on effectively communicating your firm’s value proposition and path to profits. Investors, now more than ever, want – and expect – to hear where the market opportunity lies and the unique scientific offering provided before writing a check. To secure funding, companies must be able to articulate how they will navigate FDA approval, Medicare/Medicaid reimbursement schedules, and FTC scrutiny in the post-Dobbs Decision, post-COVID world. As our Life Sciences Outlook 2023 notes, that includes “building a robust bank of knowledge” to “illustrate the market value and scientific rigor in a communications-ready format,” as well as “survey[ing] the landscape for where meaningful wins can be achieved and where serious political and reputational blows are likely to come.”
Policymakers vs. Profits Takes Center Stage
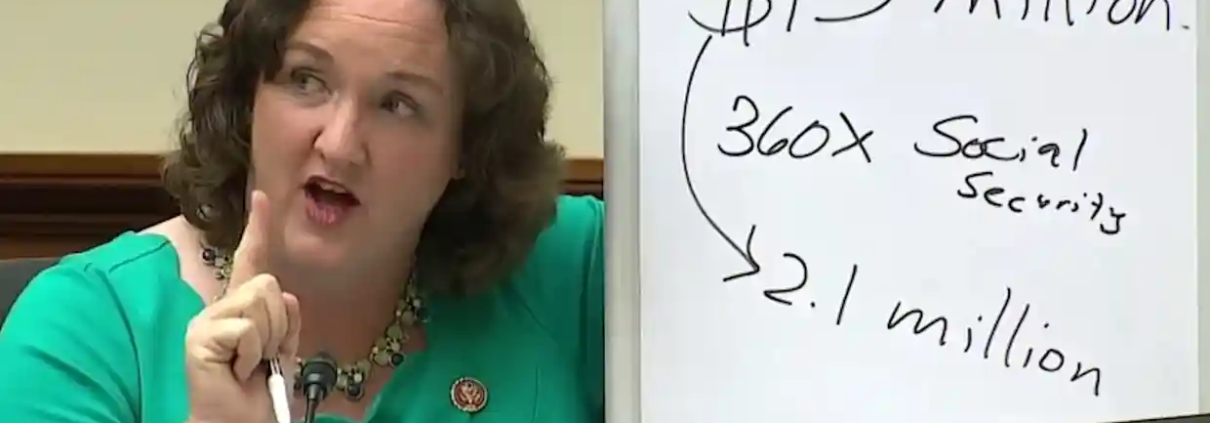
While the Inflation Reduction Act is a boon for clean energy investments, it is a major dampener for life sciences, as the bill made the long-sought goal of Medicare drug price negotiations a reality. Getting added to the Medicare reimbursement schedule is a key milestone for early-stage drug and device developers, which makes the Centers for Medicare and Medicaid Services (CMS) plan to target the first ten drugs to be negotiated by September 1st a worrisome prospect for firms and investors alike.
Already, big firms like Bristol Myers Squibb and Merck, as well as several Washington trade groups, have filed suit to stop CMS’ plan. Meanwhile, one cancer treatment innovator is weighing “slow-walking” new treatments to avoid the anticipated Medicare price pressures. Even as it complicates life sciences innovation, a new study questions whether these negotiations will actually save patients or the government any money.
Beyond the IRA’s impact, the drug pricing debate has not been put to bed. The White House continues to call for price caps and attacks pharmaceutical companies for making a profit, while some on Capitol Hill question their patent protections. Being “proactive in making the case for the unmet need you are addressing and the clinical and technological efficacy your product or technology offers” is crucial to weathering this storm.
The Pressure Won’t Stop At Price
While who pays how much for which drugs remains a fraught debate, it is not the only scrutiny from Washington and beyond. Both established and early-stage life sciences firms face new or heightened scrutiny from across the political spectrum on a range of other issues, including drug shortages and supply chain difficulties that could soon be exacerbated by pharmaceuticals’ dependency on China amidst fraying economic relations between the U.S., the EU, and China.
Life science firms must also consider regulators’ impact on strategic acquisitions, with both Washington and Brussels taking a more active approach to anti-trust enforcement. Federal Trade Commission Chair Lina Khan said the commission’s focus is cracking down on acquisitions of companies with drugs that are already on the market, such as the body’s recent lawsuit to block Amgen’s takeover of Horizon Therapeutics, but claimed the FTC recognizes newer drugs or treatments may need M&A to reach full commercialization. This view, however, did not stop the FTC from working with their European counterparts to block Illumina’s acquisition of early-stage cancer diagnostics developer Grail.
Firms also have to contend with new areas of political scrutiny driven by the twin tides of populism and progressivism, both of which are skeptical if not hostile to business. On the Left, healthcare companies have drawn ire from climate activists over greenhouse gas emissions in their supply chains and single-use plastics. On the Right, even former champions of public health research funding are now calling for those budgets to be slashed and for Congress to increase scrutiny of the industry in the wake of the politicized COVID-19 vaccine debate. In addition, lines are beginning to be drawn in the sand over the industry’s adoption of artificial intelligence. These new fronts of debate each carry serious reputational risk requiring firms to be well-versed with the full spectrum of policymakers and outside stakeholders shaping the battlefield. debates.
To Thrive, Research Can’t Just Be Relegated to the Lab
Economic concerns and increased scrutiny from regulators are leading to a tighter funding environment. To ensure life sciences firms can survive and thrive this new reality, public affairs professionals must have the right insights to avoid the regulatory and reputational roadblocks to commercial success. That means understanding the risk environment and which stakeholders and policymakers are shaping it in what ways, then diving deep to understand those actors – who can be an ally and whose efforts will your firm have to overcome? At Delve, we use this proven playbook to help firms navigate the headwinds in life sciences and beyond to further innovation and ensure commercial success.